A Miracle Baby, Not Brought About By Modulators

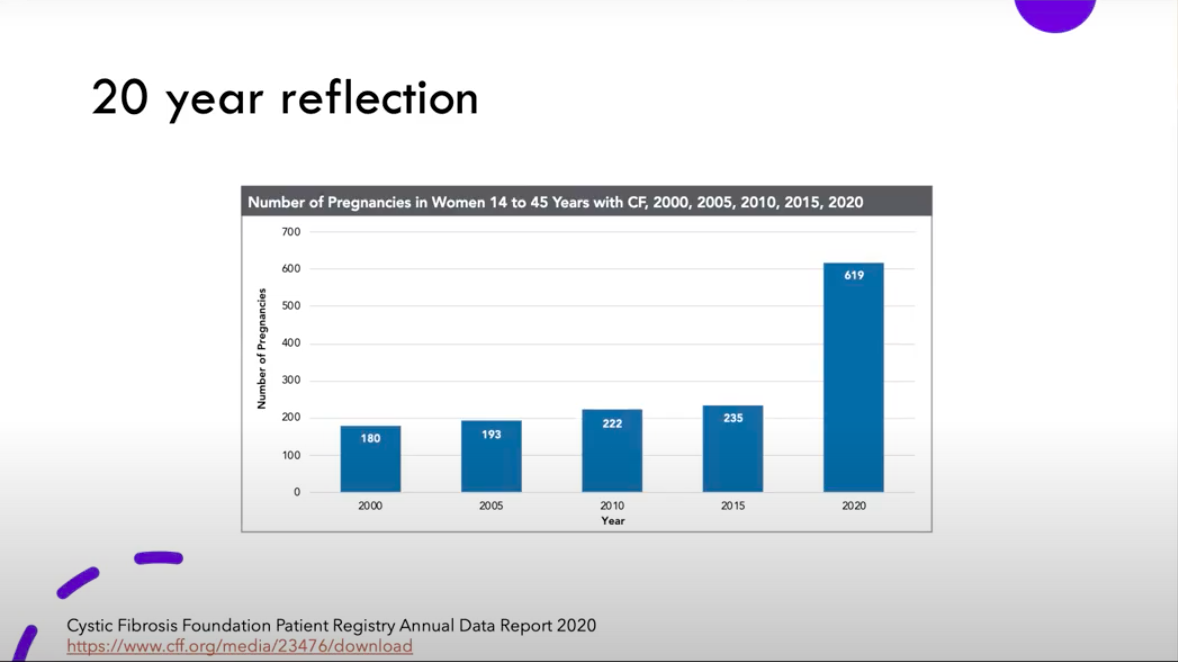
In the Dating & Relationship PTF meeting, Dr. Christon shared data from the Cystic Fibrosis Foundation’s Patient Registry, showing a dramatic increase in women with CF experiencing pregnancy in the past five years or so. This wave of so-called, “miracle babies” is mostly due to the emergence of modulator therapy. But “miracle babies,” have been happening in the CF community for much longer. CFReSHC’s own social media manager, Alicia Casals, shared her story with us this month.
Alicia grew up thinking she would never live past 30 years old, and she says she’s still shocked that she’s married and living a “normal” life with her family. Alicia married her husband, Henry, in her twenties. Early in their marriage, the couple discussed adoption or surrogacy as options for bringing a child into their family, but they never pursued this option. A few years later, when Alicia was 28, she started noticing more people with CF having babies and “not dying after or needing transplants.” It was her understanding that having a baby would greatly jeopardize her health, and that was very much the prevailing message from healthcare providers at the time — most CF doctors would warn women against pregnancy because of the potential strain it would put on their CF bodies.
Convinced their advice might be changing with the times, Alicia asked her team about it. They told her that she was “healthy enough” on their end, but wanted her to be checked out by a high risk obstetrician. Once that provider signed off, Alicia and Henry began planning for a child.
After considering the options of adoption or conception, the couple decided that whether or not they would try, would depend upon the results of Henry’s genetic carrier test. He was not a carrier, so the couple tried to conceive for a year, and nothing happened. Alicia’s high risk obstetrician provided her with a non-steroidal fertility medication, clomiphene. The medication causes the pituitary gland to release the hormones that are needed to stimulate the release of eggs from the ovaries. She pursued this option for two cycles, and still nothing happened. Then she connected with an infertility specialist, underwent various tests, and was informed that “everything looked fine.” The provider brushed the issue off, saying, “it’s just your CF.” After all of that, Alicia and Henry decided to pay out-of-pocket for three intrauterine inseminations (IUI), and still nothing happened. At this point, the couple decided to transfer to a doctor who had previously cared for CF patients.
For years, Alicia had told her healthcare providers that her periods were horrible, painful, inconsistent, and exhausting. She was pretty convinced that she had Polycystic Ovary Syndrome or endometriosis, but was never examined for either. After describing her issues to this new doctor, Alicia was told that she was probably right. After some testing to confirm, she underwent a surgery to remove endometriosis tissue and a few cysts. They then decided to try IUI again, and after three tries, still nothing happened. Next, they decided to try IUI three more times, with stronger support medications. Alicia underwent one round, and decided that she needed a break. She was exhausted; it had been a long journey.
Alicia’s experience with this doctor changed everything. Women deserve to be heard by their providers — instead of being dismissed, misdiagnosed, neglected, and even gaslighted. Alicia’s experience is unique, but at the same time, very familiar.
Can you guess how her “miracle baby” story ends? It ends with a cessation of all medications and procedures, followed by a surprise, unassisted conception of her daughter, Lola. Alicia was ecstatic. Now, four years later, in 2022, she is still shocked.
Alicia’s first trimester was rough. She dealt with nausea, extreme fatigue, and major anxiety. She had experienced depression before, but had never lived through the emotional turmoil that is a depression-anxiety mix. She spent a lot of time in bed.
Other than that, her pregnancy went without complications. At 39 weeks, Alicia and her doctors decided to induce labor. That process went on for 24 hours, before Alicia finally asked about a cesarean section (c-section) surgery. Alicia shared that she was scared of a vaginal birth, and that as a CF patient, she was accustomed to surgeries and less scared of a c-section. The team appeased her wishes with the surgery, and discovered that the baby was so high up that they needed to use a vacuum to assist with the delivery.
Finally, after years of trying, Alicia and Henry brought their “miracle baby,” Lola, into the world.