Heart Health
CFReSHC CF-SRH Resource Guide by Patients for Providers and Patients
Key
For Providers
For Patients
For Patients and Providers
Introduction
As advancements in treatment extend the lives of people with cystic fibrosis (CF), a new set of health concerns has come into focus. One of the most critical concerns is cardiovascular health. CF has been primarily considered a lung and digestive disease, but emerging research shows that the heart is also significantly affected [Poore, Frost, Eising, Sandouk]. This evolving understanding calls for a more comprehensive approach to CF care that proactively monitors and manages heart health alongside traditional CF concerns.[1–3]
 Cardiovascular complications are becoming more common in the CF population as patients live longer and therapies improve.[1,2] These complications may stem not only from the effects of chronic lung disease but also from systemic factors such as inflammation, oxidative stress, and the specific biology of CF itself. Studies have shown that the CFTR protein is expressed in the cardiovascular system, particularly affecting the left side of the heart.[3,4] This has been linked to cardiomyopathy and other cardiac abnormalities.[3–7]
Cardiovascular complications are becoming more common in the CF population as patients live longer and therapies improve.[1,2] These complications may stem not only from the effects of chronic lung disease but also from systemic factors such as inflammation, oxidative stress, and the specific biology of CF itself. Studies have shown that the CFTR protein is expressed in the cardiovascular system, particularly affecting the left side of the heart.[3,4] This has been linked to cardiomyopathy and other cardiac abnormalities.[3–7]
Age-related heart disease is already the leading cause of death in the general U.S. population [CDC], and people with CF may face unique risks due to:
- Chronic systemic inflammation and CFRD: Ongoing inflammation, combined with CF-related diabetes (CFRD), can contribute to the development of atherosclerosis and increase susceptibility to coronary vascular disease (CVD).[6]
- High blood pressure: Elevated blood pressure may damage arteries and limit oxygen supply to the heart, compounding the cardiovascular strain.[6]
Some studies suggest that even in the absence of diagnosed pulmonary hypertension, people with CF may experience early changes in heart structure and function and oxidative stress, which can impair the heart’s ability to contract and relax properly.[2,8] This may help explain findings such as increased diastolic blood pressure and elevated heart rates in CF patients.[2,8]
Another possible contributor is subclinical pulmonary hypertension, temporary, often undetected increases in lung pressure that, over time, may damage the right ventricle of the heart, even in well-controlled CF cases.[8]
These factors emphasize the importance of early detection and management of cardiovascular issues in CF. As one study emphasizes, “More awareness is needed for the prevention and treatment of CVD in the aging CF population to reduce the future comorbidities that may be related to untreated cardiovascular disease.”[9]
By promoting education, lifestyle changes, and regular cardiovascular monitoring, people with CF and their care teams can begin to address this emerging aspect of long-term health with greater confidence and clarity.
- How many calories are you eating per day? [If they do not know already, patients can work with a dietitian to determine how many calories they consume daily.]
- How much salt (mg) are you eating per day? [If they do not know already, patients can work with the dietitian to determine how much salt they consume daily.]
- How much exercise do you get per day?
- Do you smoke/vape or participate in recreational drugs?
- What is your CFRD status?
- Modulator status?
- Screen patients for anxiety, depression, or other mental health concerns.
- Do you currently work out?
- If not, would you like to know how exercise can lower your risk of heart disease?
- Suggest an exercise program or pulmonary rehabilitation for those with advanced lung disease.
- Am I at risk for heart-related issues due to my CF?
- What can I change today to lower my risk of heart disease?
- What is the best way to start an exercise program?
- How do I measure my salt intake?
- How can I track my calorie intake?
- What are some ways to improve my mental health, and how will this help my heart health?
Cardiovascular Risk Factors with CF
Managing more complex health needs and understanding and monitoring cardiovascular risk are crucial for pwCF to live longer. Ongoing inflammation, metabolic changes, and the evolving effects of modulator therapy play a role in cardiovascular changes. Early and accurate diagnosis using advanced imaging tools and monitoring for emerging risk factors can improve long-term outcomes.
Several overlapping factors may contribute to increased heart disease risk in people with CF:
-
- Chronic Inflammation and Metabolic Stress
Systemic inflammation can contribute to endothelial dysfunction and increase the risk of coronary vascular disease.[10] This is especially significant in individuals who also have CF-related diabetes (CFRD), which affects over half of the CF population and becomes more common with age.[10,11] Plaque buildup and abnormal glucose metabolism in CFRD further raise the risk of heart disease.[10,12] - Nutrition and Dietary Influence
Historically, people with CF have been encouraged to consume a high-sodium diet to compensate for salt loss through sweat.[13] However, excessive sodium intake may contribute to long-term cardiovascular strain, particularly as patients age and their nutritional status improves.[3,11,12] - Weight Gain and Obesity
With the success of CFTR modulators, many individuals are experiencing increased appetite and improved nutrient absorption, leading to unintentional weight gain and, in some cases, obesity.[3,11,12] This can increase mortality overall; however, excess weight is also a known risk factor for cardiovascular disease.[10,11] - Mental Health and Lifestyle Factors
Mental health challenges, including anxiety, depression, and PTSD (post-traumatic stress disorder), are prevalent in the CF population and may indirectly affect heart health through stress pathways.[10,12] Lifestyle behaviors such as smoking or vaping can further increase cardiovascular risk.[3,10] - Blood Pressure and Vascular Health
High blood pressure, whether due to systemic inflammation, vascular stiffness, or other metabolic changes, can damage arteries and impair oxygen delivery to the heart.[3,12] Monitoring for hypertension is essential, especially in patients with additional co-morbidities.[10]
- Chronic Inflammation and Metabolic Stress
- Diagnostic Tools to Identify Cardiac Changes in CF
Diagnosing heart health issues is detrimental to people with CF since cardiovascular complications can often be overlooked.[6,8,10] Especially since symptoms such as fatigue or shortness of breath can mimic complications from respiratory infections and advancement of the disease.[3,8,10,14] Identifying heart complications in CF requires advanced imaging tools to discover the correct diagnosis promptly.
Right Heart Evaluation
Assessing the right ventricle (RV), which is often affected by CF-related lung disease, can be complex due to its crescent shape and unique structure.[15] Traditional echocardiography methods used for the left side of the heart are less accurate for RV assessment. However, newer technologies such as tissue Doppler imaging (TDI) and speckle-tracking echocardiography (STE) offer more precise evaluation of proper heart function in CF.[15]
Advanced Imaging Techniques
Speckle-tracking echocardiography can detect subclinical right and left ventricular dysfunction even before symptoms develop.[6] This has proven valuable in identifying early cardiomyopathy across various conditions.[6,8] Cardiac MRI provides a detailed look at overall heart structure and physiology, aiding in comprehensive cardiovascular assessment.[16]
Pulmonary Hypertension and Cor Pulmonale
Cor pulmonale, or right heart failure secondary to lung disease and pulmonary hypertension, is one of the most common cardiovascular complications in CF.[14,16] Both conventional and tissue Doppler echocardiography have revealed structural and functional changes in the right heart, and modern STE has detected even earlier signs of dysfunction.[14]
Bronchiectasis and Heart Changes
One study focused on people with CF who have bronchiectasis, a condition characterized by scarring, frequent infections, and chronic inflammation of the airways. Using speckle-tracking echocardiography, researchers identified functional changes in the right atrium and right ventricle and thickening of the pulmonary artery walls.[14] Notably, the severity of bronchiectasis was significantly correlated with pulmonary artery wall thickness, suggesting this could become a useful diagnostic marker in the future.[14]
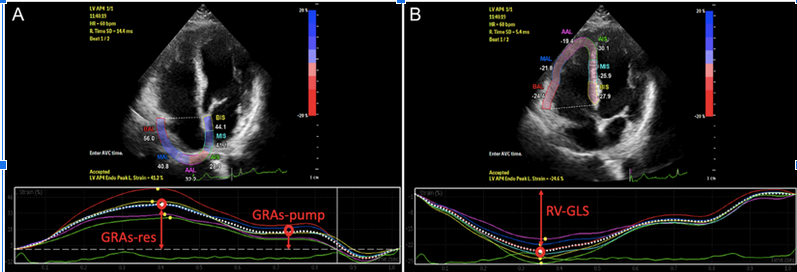
Figure 1. Right ventricular global longitudinal strain (RV GLS), global longitudinal right atrial strain during ventricular systole
(GRAs-res), and global longitudinal right atrial strain during late diastole (GRAS-pump) were measured by speckle-tracking
echocardiography analysis of 6 consecutive myocardial segments in the RV and the RA.[14]
Obesity and Nutritional Aspects with CF and Heart Health
Historically, people with CF were encouraged to consume high-calorie, high-fat diets to combat malabsorption and increased metabolic demands.[17,18] This strategy helped to improve mortality. However, the introduction of CFTR modulators has significantly altered nutritional outcomes while changing dietary goals, and new risks have developed.[3,19]
As of 2021, nearly one-third of adults with CF were considered overweight or obese.[17] This trend is partially attributed to improved nutrient absorption and increased appetite associated with modulator therapy.[19] While better absorption is a positive advancement, it raises new concerns, such as the unknowns around fat-soluble vitamin uptake [Swetland] and the unintended acceleration of conditions like atherosclerosis and obesity.[3,17,19]
Obesity, once rare in the CF population due to chronic malabsorption, is now emerging as a clinical issue. This reflects trends in the general population, where overweight and obesity are well-established risk factors for cardiovascular disease, including systemic hypertension and ischemic heart disease.[3,18,20,21]
Sodium intake is another shared concern between CF patients and the general population. A high-sodium diet was once a standard for CF patients due to excess salt loss through sweat.[18] However, excessive sodium consumption can contribute to cardiovascular strain. It may no longer be appropriate for all individuals with CF, especially those now achieving normal or higher BMIs on modulators.[1,11,18]
Despite these evolving risk factors, atherosclerosis has historically been rare in CF patients, particularly in those with pancreatic insufficiency.[3,11] One hypothesis suggests that chronic fat malabsorption leads to persistently low LDL cholesterol levels, which may protect against plaque buildup in arteries.[3,11] However, rising evidence indicates that CF patients without pancreatic insufficiency might still be susceptible to atherosclerotic changes, especially in modulator-induced weight gain and diet shifts.[3]
These findings stress that CF nutrition is no longer a set menu for all. Individual genetics, modulator use, pancreatic function, and cardiovascular risk must all be considered when planning dietary and nutritional strategies.[3]
There is also growing interest in the role of micro-nutrient deficiencies, such as selenium, and their potential link to cardiac issues in CF.[6] While some case studies have pointed to a possible association between selenium deficiency and cardiac dysfunction, more research is needed to confirm whether supplementation could help reduce heart-related complications.[3,6] Genetic differences may make some individuals susceptible to these deficiencies and their cardiac effects.[6]
Overall, the nutritional landscape in CF is shifting. With increased longevity and modulator use, there’s a need for updated, individualized approaches to diet and weight management, especially considering the growing concerns of cardiovascular health.
Ways to Decrease Cardiovascular Risk with CF
People with cystic fibrosis (CF) can take active steps to lower their risk of heart-related complications. Speaking with your CF pulmonologist, dietitian, or care team about personalized strategies is essential. While recommendations will vary based on individual health status, several general approaches are supported by research and clinical experience. However, do not change anything without consulting your CF care team first.
Build an Exercise Routine
A structured exercise regimen is one of the most effective ways to support cardiovascular health. People with CF are encouraged to work with their care team to create an exercise plan that fits their abilities and goals. In particular:
-
- Ask your CF care team about including a physical therapist to guide you in developing a safe and effective program.
- Consider participating in a supervised pulmonary rehabilitation program to help begin or enhance your fitness journey.
- Use a fitness or wearable activity tracker (WAT) to monitor your daily activity and stay motivated.
Exercise training (ET) is widely recommended as part of CF treatment to help maintain respiratory function, improve physical fitness, and enhance quality of life [Anifanti]. Wearable activity trackers have also supported CF’s adherence to structured exercise programs. These tools may offer a practical way to improve daily movement and gain insight into physical progress.[7]
Regular exercise, however, has been shown to promote improvements in lung function, endurance, and mental health.[7] Although fewer studies have directly addressed the role of exercise in cardiac outcomes, some findings suggest that individuals with higher physical activity levels experience clearer cardiac adaptations, particularly in right ventricular (RV) function.[7]
Despite its known benefits, more research is needed to determine the most effective and safest exercise and its specific impact on heart function in CF.[7]
Many people with CF experience reduced physical activity due to breathing difficulties, muscle weakness, and heart dysfunction (in advanced lung disease).[7] These limitations can lead to a sedentary lifestyle, which may worsen overall health and increase the risk of complications.[7]
By engaging in regular, tailored physical activity, people with CF may reduce their risk of heart complications while improving their health and quality of life. Ongoing collaboration with the care team is key to designing a sustainable, effective exercise plan.
Cardiovascular Health and CF-Related Diabetes (CFRD)
Cystic fibrosis–related diabetes (CFRD) is the most common non-pulmonary complication in people with CF and is increasingly recognized as a contributor to cardiovascular concerns.[11]
The general population shows a link between diabetes and cardiovascular disease, which also appears and shares similar risks in the CF population.[4,11] Chronic hypoxia from CF can lead to left ventricular dysfunction, and when combined with hyperglycemia, may contribute to the development of cardiomyopathy.[4] Over time, this can progress to myocardial fibrosis and pulmonary hypertension, further increasing cardiac risk.[4]
Connected Risk Factors
As life expectancy in CF continues to rise, cardiovascular health is becoming a greater concern. People with CF are experiencing changes in body weight, lipid levels, and systemic inflammation.[5] These factors are associated with both diabetes and cardiovascular disease.[5] CFTR modulator therapy has further altered the nutritional picture by improving fat absorption, which can lead to elevated cholesterol and weight gain.[3,5,22] These changes may heighten the risk for heart strain and hypertension, particularly in individuals with CFRD.[5,22]
CFRD shares characteristics with both type 1 and type 2 diabetes. While insulin deficiency is common, insulin resistance and altered fat metabolism also play a role, making cardiovascular complications a growing concern.[5]
What to Consider
These trends highlight the importance of cardiovascular monitoring in CF care, particularly for individuals with longstanding CFRD or other known risk factors. Key questions remain, such as:
-
- When and how should clinicians screen for cholesterol and other cardiovascular markers?
- When should cholesterol-lowering treatments be considered?
- How do these interventions interact with existing CF therapies?
More research is needed to develop clinical guidelines, but early attention to symptoms like chest pain, shortness of breath, or unexplained fatigue may help identify heart-related complications sooner.[22]
As the landscape of CF care evolves with modulator therapy, cardiovascular risk in CFRD should not be overlooked. Monitoring and personalized care with the CF Pulmonology and endocrinology team will be essential for maintaining long-term heart health in this growing adult population.[22] Individuals should monitor blood glucose as advised and consistently take prescribed CFRD medications.
Mental Health and Impact on Heart Health
Extensive research shows there is a connection between mental health and heart health.[20,23–25] This creates a whole new facet to treating and diagnosing depression and/or heart disease. Together, mental health and heart health lead to a general decline in people suffering.[23,24]
People experiencing mental health issues such as depression, anxiety, stress, and even post-traumatic stress disorder (PTSD) over a long period may experience specific side effects such as increased cardiac reactivity (e.g., increased heart rate and blood pressure), reduced blood flow to the heart, and heightened levels of cortisol.[20,23,24] Over time, these physiologic effects can lead to calcium buildup in the arteries, metabolic disease, and heart disease, which can cause heart attack, stroke, and heart failure.[20,23,25]
Studies are correlating the risk of depression with heart disease, whether it be hypertension or heart failure.[23,24] Acknowledging the condition of the heart in depression, anxiety, or other mental health sufferers is vital in helping maintain a good heart health regimen.[23]
The Mental Stress of Cystic Fibrosis with the Heart
People with Cystic Fibrosis have an extensive daily medical regimen. This can involve hours of breathing treatments, taking handfuls of medications, inhalers, and sinus rinses, and trying to have a professional and social life. If a person with CF is already struggling with anxiety and depression, they’re less likely to make healthy decisions.[23] This means they are more likely to skip or not take their medication, sleep too much or too little, and be physically inactive. Over time, this can lead to unhealthy habits, affecting the heart.[23]
Ways to Keep the Balance on Heart Health and Mental Health
Psychological interventions have been shown to help mitigate anxiety, depression, and negative feelings in people affected by poor heart health.[24] Various techniques for these interventions, such as cognitive behavioral therapy (CBT), eye movement desensitization and reprocessing (EMDR), social cognitive therapy, and motivational interviewing, are just a few listed that can provide a mental reprieve for heart disease sufferers.[24]
Pharmacological interventions remain as high options along with the psychological interventions previously mentioned.[24,26] Over the past several decades, advancements in pharmacology for depression have brought about many treatment options for mental health.[26]
What the CF Care Team Can Do
The longevity that medical advances have placed on people with CF has shown that medical issues once deemed safe are now having long-term side effects. People with CF should be offered and assessed as to their mental health regardless of heart health; however, knowing the correlation between these two health conditions, seeking the care of a cardiologist is recommended if circumstances require adding this provider to your care team. Assessing mental health using the DSM-5 or other surveys established within the care team’s medical practice is essential during clinic visits. Addressing mental health issues can lead to better outcomes, positively affecting heart health.
Modulators and Heart Health
While lung complications have historically been the leading cause of mortality in people with cystic fibrosis (CF), the introduction of CFTR modulator therapies has significantly extended life expectancy and shifted the landscape of long-term health outcomes.[11] New concerns over cardiovascular health are beginning to emerge as areas needing attention and research.
CFTR modulators, such as elexacaftor/tezacaftor/ivacaftor (ETI), work by correcting the underlying protein defect in CF. These treatments improve lung function and enhance nutrient absorption, contributing to better overall health and nutritional status in people with CF.[3] However, their effects on other organ systems are still being explored, and evidence about their full impact remains limited.[11,21]
Recent reports suggest that these therapies may influence cardiovascular health in ways not yet fully understood. In several case observations, individuals (primarily women with pre-existing metabolic conditions like CF-related diabetes (CFRD) or liver disease) developed cardiovascular changes after starting ETI therapy. These findings raise important questions about how restored CFTR function might interact with metabolic and hormonal pathways.[10,21]
Although severe arterial hypertension (SAH) has not been documented in large clinical trials, the pattern of case reports underlines the importance of monitoring cardiovascular markers, particularly in those with known CV risk factors.[10,21]
As modulator therapy continues to evolve, it may benefit care teams to assess baseline cardiovascular health. This would include blood pressure and blood sugar tests before initiating treatment.[10,21] These case studies warrant further research into the broader, extra-pulmonary effects of CFTR modulators. Future in vitro and clinical studies could help clarify how CFTR correction influences heart function and other organ systems beyond the lungs.[21]
Lung Transplant
As people with cystic fibrosis (CF) live longer, more are reaching advanced stages of lung disease and may require lung transplantation. With this progression comes a greater focus on cardiovascular health, particularly regarding transplant readiness and long-term outcomes.
In advanced CF, the heart, especially the right ventricle, can become strained due to prolonged low oxygen levels (hypoxemia) and high levels of carbon dioxide (hypercapnia).[5,16] This chronic stress can lead to structural and functional changes in the heart, such as:
-
- Right ventricular dysfunction and cor pulmonale: a condition caused by high blood pressure in the lungs (pulmonary hypertension) that increases the workload on the right side of the heart.[5,16]
- Heart muscle thickening (hypertrophy), myocardial fibrosis (scarring), and reduced pumping efficiency: possibly linked to chronic inflammation, electrolyte imbalances, and CF-related disruptions in salt and fluid regulation.[5,16]
Cardiac Considerations in Lung Transplantation
Despite the availability of CFTR modulators, lung transplants remain necessary for many individuals. Some patients cannot tolerate modulators or have rare genetic mutations that make them ineligible for these therapies.[19] As the disease advances, complications involving other organs, especially the heart, can arise, influencing transplant eligibility and outcomes.[16,19]
During transplant evaluation, cardiovascular health plays a critical role. Increased pulmonary pressures can cause or worsen right heart dysfunction as the lungs deteriorate. Additionally, symptoms like fatigue and breathlessness, commonly seen in both heart and lung disease, can make it challenging to distinguish cardiac involvement without proper screening.[5]
Routine cardiac assessments, including imaging and functional tests, are essential for identifying heart issues early and ensuring individuals are medically optimized for transplant.[5]
Post-Transplant Heart Health Concerns
Cardiovascular complications may persist or even emerge after transplantation. Research has shown that:
-
- Atrial arrhythmias are relatively standard following lung transplant procedures.[3]
- Other post-operative issues include pulmonary artery stenosis or kinking, anastomotic complications, pulmonary embolism, and vascular abnormalities.[3]
- These complications can be influenced by pre-existing heart strain from CF and the transplant surgery itself.[3]
Patients are encouraged to discuss heart-related risks with their transplant pulmonologist and cardiovascular team to understand individual risk factors and monitoring plans.
Peer to Peer Advice
- Include forms of cardiovascular exercise in your exercise routine (e.g., walking, biking, stationary bike, hiking, tennis, team sports, etc.)
- Keep track of your blood pressure. Having a home blood pressure monitor helps check your blood pressure. Address high blood pressure by consulting a cardiologist or internist.
- Free apps can track calories, weight, and fitness (separately or in combination). Consider using them to monitor preventive measures to protect your heart health.
- If using an app to track your health, sharing the data with your provider is essential.
Works Cited
- Frost F, Nazareth D, Fauchier L, et al. Prevalence, risk factors, and outcomes of cardiac disease in cystic fibrosis: a multinational retrospective cohort study. Eur Respir J. 2023;62(4):2300174. doi:10.1183/13993003.00174-2023
- Eising JB, Van Der Ent CK, Teske AJ, Vanderschuren MM, Uiterwaal CSPM, Meijboom FJ. Young patients with cystic fibrosis demonstrate subtle alterations of the cardiovascular system. J Cyst Fibros. 2018;17(5):643-649. doi:10.1016/j.jcf.2017.12.009
- Poore TS, Taylor-Cousar JL, Zemanick ET. Cardiovascular complications in cystic fibrosis: A review of the literature. J Cyst Fibros. 2022;21(1):18-25. doi:10.1016/j.jcf.2021.04.016
- Shah PH, Lee JH, Salvi DJ, Rabbani R, Gavini DR, Hamid P. Cardiovascular System Involvement in Cystic Fibrosis. Cureus. Published online July 29, 2021. doi:10.7759/cureus.16723
- Duus LS, Dons M, Thudium RF, et al. Cardiac Structure and Function in People with Cystic Fibrosis. J Cyst Fibros. 2024;23(6):1138-1145. doi:10.1016/j.jcf.2024.09.012
- Segovia-Cubero J, Ruiz-Bautista L, Maiz-Carro L, et al. The cardiomyopathy of cystic fibrosis: a modern form of Keshan disease. Front Cardiovasc Med. 2024;11:1285223. doi:10.3389/fcvm.2024.1285223
- Anifanti M, Giannakoulakos S, Hatziagorou E, et al. Effects of a Long-Term Wearable Activity Tracker-Based Exercise Intervention on Cardiac Morphology and Function of Patients with Cystic Fibrosis. Sensors. 2022;22(13):4884. doi:10.3390/s22134884
- Sciatti E, Vizzardi E, Bonadei I, et al. Focus on echocardiographic right ventricular strain analysis in cystic fibrosis adults without cardiovascular risk factors: a case–control study. Intern Emerg Med. 2019;14(8):1279-1285. doi:10.1007/s11739-019-02104-5
- Ticona JH, Lapinel N, Wang J. Future Comorbidities in an Aging Cystic Fibrosis Population. Life Basel, Switzerland. 2023;13(6):1305. doi:10.3390/life13061305
- Saunders T, Burgner D, Ranganathan S. Identifying and preventing cardiovascular disease in patients with cystic fibrosis. Nat Cardiovasc Res. 2022;1(3):187-188. doi:10.1038/s44161-022-00030-y
- Sandouk Z, Nachawi N, Simon R, et al. Coronary artery disease in patients with cystic fibrosis – A case series and review of the literature. J Clin Transl Endocrinol. 2022;30:100308. doi:10.1016/j.jcte.2022.100308
- Despotes A. CF and Cardiovascular Disease: Listen to your Heart! https://cfri.podbean.com/e/alex-d-video/
- Cystic Fibrosis Foundation. Minerals. https://www.cff.org/managing-cf/minerals#:~:text=Not%20getting%20enough%20salt%20can,especially%20during%20hot%2C%20humid%20weather
- Gürel E. The Impact of Cystic Fibrosis- and Noncystic Fibrosis-Bronchiectasis on Pulmonary Artery Wall Thickness and Right Heart Functions Assessed by Speckle-Tracking Echocardiography. Anatol J Cardiol. Published online 2023:319-327. doi:10.14744/AnatolJCardiol.2023.2864
- Ozcelik N, Shell R, Holtzlander M, Cua C. Decreased Right Ventricular Function in Healthy Pediatric Cystic Fibrosis Patients Versus Non-Cystic Fibrosis Patients. Pediatr Cardiol. 2013;34(1):159-164. doi:10.1007/s00246-012-0407-4
- Temur HO, Alkan A, Yozgat CY, et al. MRI evaluation of right heart functions in children with mild cystic fibrosis. Cardiol Young. 2023;33(10):1828-1833. doi:10.1017/S1047951122003249
- Kutney KA, Sandouk Z, Desimone M, Moheet A. Obesity in cystic fibrosis. J Clin Transl Endocrinol. 2021;26:100276. doi:10.1016/j.jcte.2021.100276
- Litvin M, Yoon JC, Casella JL, Blackman SM, Brennan AL. Energy balance and obesity in individuals with cystic fibrosis. J Cyst Fibros. 2019;18:S38-S47. doi:10.1016/j.jcf.2019.08.015
- Swetland DV, Savant AP. Cystic fibrosis year in review 2023. Pediatr Pulmonol. 2024;59(12):3106-3116. doi:10.1002/ppul.27190
- Centers for Disease Control. About Heart Disease and Mental Health. May 15, 2024. https://www.cdc.gov/heart-disease/about/about-heart-disease-and-mental-health.html
- Gramegna A, De Petro C, Leonardi G, et al. Onset of systemic arterial hypertension after initiation of elexacaftor/tezacaftor/ivacaftor in adults with cystic fibrosis: A case series. J Cyst Fibros. 2022;21(5):885-887. doi:10.1016/j.jcf.2022.04.010
- Thambuluru SR, Kyazimzade S, Despotes KA, Kirk D, Goralski JL. Acute ST-elevation myocardial infarction in two young women with cystic fibrosis and cystic fibrosis-related diabetes. J Cyst Fibros. 2022;21(1):e44-e47. doi:10.1016/j.jcf.2021.11.013
- Santoni S, Kernic MA, Malloy K, et al. Depression and Incident Hypertension: The Strong Heart Family Study. Prev Chronic Dis. 2025;22:E06. doi:10.5888/pcd22.240230
- Ski CF, Taylor RS, McGuigan K, et al. Psychological interventions for depression and anxiety in patients with coronary heart disease, heart failure, or atrial fibrillation: Cochrane systematic review and meta-analysis. Eur J Cardiovasc Nurs. 2025;24(2):194-204. doi:10.1093/eurjcn/zvae113
- American Heart Association. How Does Your Mental Health Affect the Heart? https://www.heart.org/en/healthy-living/healthy-lifestyle/mental-health-and-wellbeing/how-does-your-mental-health-affect-the-heart
- Apostolos A, Konstantinou K, Ktenopoulos N, et al. Depression and Coronary Artery Disease—Where We Stand? J Clin Med. 2025;14(12):4281. doi:10.3390/jcm14124281
Free Printable PDF Download
Want a free printable PDF download of this section for your use in clinic? Just give us your name and email address below to get your download link. This will not add you to our email list.