Menopause
the final menstrual period, determined after 12 months with no vaginal bleedingCFReSHC CF-SRH Resource Guide by Patients for Providers and Patients
Key
For Providers
For Patients
For Patients and Providers
Introduction
The menopausal transition (MT) is the period between the premenopause stage and the final menstrual period (FMP). It is a gradual process that occurs over several years as ovarian reproductive function declines, leading to the end of menstrual cycles.[1] Though many people use MT and perimenopause interchangeably, perimenopause is slightly different; it covers the same period as the menopausal transition but also includes the point of menopause (which is 12 months after the FMP).[2] The average length of perimenopause is four years, but it can last from several months to ten years.[3]
The MT usually begins in the mid to late 40s in the general population, and the average age at which women in the general population reach menopause is 52.[4] A 2009 abstract by Tsang, however, noted the the average age of starting the MT for women with CF was 37.8 years, with menopause reached at an average age of 47.8 years.[5] This is about four to nine years younger for the MT than the general population, and four years younger for menopause. A more recent Prochownik survey, published in 2023, found that females with CF reached menopause only 2-3 years earlier than the general population.[6,7] This data aligns with the finding that earlier ages of menopause (compared to the general population) are common for women with chronic diseases.8 The slightly smaller gap between the Tsang and Prochownik data is likely due to new CF therapies and better health among females with CF, though further study is needed.
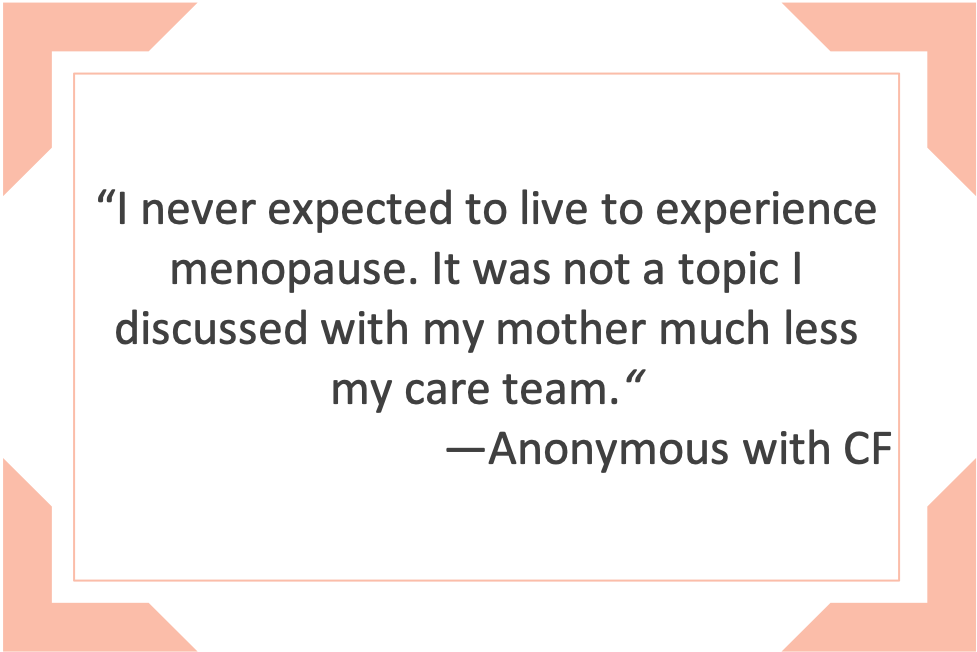
Unfortunately, discussions in the CF clinic about menopause are rare. Only 1% of participants in Prochownik’s study reported discussing menopause with their CF provider, even though 19% expressed interest in talking about it with their CF team.[7]
Menopause in CF is not a well-researched topic, because until recently, very few patients lived long enough to reach menopause. With better treatment options, patients are surviving longer, and more women with CF are entering this life phase. In the average life span, women will spend one-third of their life in menopause. Menopausal physical changes on average last four years to 10 years [2]. Studies promote hormone replacement therapy during this life phase to improve quality of life [2,3]. Therefore, an exploration of menopausal symptoms and treatments warrants exploration as women with CF look to differentiate CF symptoms from peri/postmenopausal physical changes and seek treatment options.
- What is your cycle like currently– how many days between the first day of each period from one month to the next? How many days of bleeding? Are either of these a change for you?
- Are you tracking if CF symptoms vary during different phases of your menstrual cycle?
- Have you experienced symptoms of perimenopause or menopause, such as hot flashes, sleep disturbances or depression? Have you noticed changes in your sex life, menstruation, vaginal lubrication, sleep patterns, and/or mood?
- Have you discussed these changes with your OB/GYN or endocrinologist?
- Are you taking any over the counter supplements to help you through perimenopause/menopause?
- What is your family history regarding menopause? At what age did your mother start the MT? At what age did your mother reach menopause?
- How do your perimenopause symptoms impact your life? Have you made any changes to your daily routine to accommodate these symptoms?
- Which perimenopause symptom is the worst for you?
- Do you take any herbal supplements to treat your symptoms? (If yes, ask them to bring the supplements with them or share a list or photo of the supplements to include in the chart.)
Patient to CF Provider:
- My gynecologist suggests I may have started perimenopause. How will this affect my CF care?
- What should I expect after menopause and what are your recommendations for hormone therapy, herbal menopause treatments, and my CF care at this life stage?
- What hormone therapies could interact with my current medications?
- Do CFTR Modulators have any effect on perimenopause and menopause?
- Do women with CF enter menopause early?
- Can you direct me to the research being done on menopause in females with CF?
Patient to GYN provider:
- (For GYN) How does my CF care affect my hormones? Would you be willing to speak with my CF team about my issues?
- What signs and symptoms should I pay attention to relating to perimenopause or menopause?
- Is there any hormonal testing I can get to clarify which stage I am in the MT transition (early, late)?
Signs and Symptoms of (Peri)Menopause
Menopause is considered the day of a woman’s last period, defined after 365 days without menstruation. The time prior is considered perimenopause and the days following are termed post menopausal. During menopause, the sex hormones estrogen, progesterone and testosterone are reduced, which can lead to “atrophy of the vaginal mucosa, causing vaginal dryness, dyspareunia (painful intercourse), itching, vaginal stenosis and urinary incontinence” [3].
During perimenopause and menopause a variation in hormone levels can produce physiological and psychological changes. Women might experience some or all of the following:
| Variations in frequency, duration and flow of periods |
Incontinence/ Urinary tract infections |
Weight gain/slowing metabolism | Hair growth on chin, upper lip and cheeks (face) |
| Mood changes/depression/anxiety | Hot flashes/night sweats | Vaginal dryness | Painful intercourse (dyspareunia) and/or low libido |
| Interrupted sleep | Muscle tone loss | Hair loss/thinning | Osteopenia/osteoporosis |
During Menopause Transition (MT), estrogen, progesterone, follicle-stimulating hormone, luteinizing hormone, and testosterone can fluctuate significantly, causing a wide range of symptoms that affect multiple organ systems. Many of these symptoms persist in the postmenopause stage, depending on the person. Managing these symptoms can be challenging for both patients and clinicians and often impacts patients’ quality of life.[1] Symptoms can include: hot flashes, night sweats, vaginal dryness, joint pain, sleep disturbances, mood changes, brain fog, irregular periods and heavy bleeding. Females with CF may experience other CF-specific symptoms, like difficulty breathing, hemoptysis, thicker and greater amounts of sputum, and more gastrointestinal problems, to name a few.[5] Differentiating CF symptoms from those of perimenopause can be difficult, as they often overlap.[6] Prochownik et al. reported that 97% of their participants (n=39) reported at least one MT symptom. The most common symptoms included waking up early, night sweats, stiffness of joints, hot flashes, and vaginal dryness.[7] CF symptoms either became worse or did not change during (peri)menopause.[6,7] Both of these studies were conducted before the advent of CFTR modulators, however. Thus, more information is needed on the changes in menopause symptoms that have occurred for patients in the post-modulator era.
Tsang has noted the most significant reported perimenopausal changes for women with CF were sleep disturbance and depression[6]. For its part, menopause research in the general population suggests that having a history of depression makes it more likely a women will experience a depressive episode as she approaches menopause. Bromberger and Epperson (2018) recommend treating women for depressive symptoms experienced during this transitional phase and indicate that the rate of depression declines 2-4 years after the final menstrual period [7].
Implications of Menopause for Women with CF
Women who experience natural menopause before age 40 (considered early menopause) can have greater risks of adverse health outcomes, like cognitive impairment, dementia, osteoporosis, mood disorders, sexual dysfunction, and mortality.[9] Gold et al, however, found that risk is mitigated by sociodemographic factors, like level of educational attainment, being employed, not smoking, and having better self-rated health.[9]
Impact on Lung Function
Hormones fluctuate during perimenopause, which could cause frequent congestion and worsened CF symptoms.[1] A study on the impact of menopause on lung function in the general population found a decline, including accelerated decline in FVC and FEV1, as well as new onset of asthma and increased respiratory symptoms.[1]
People with CF are already at risk of more rapid bone loss (see Bone Health chapter: Bone Health in Cystic Fibrosis | CFReSHC for more information) due to a history of steroid use, nutritional issues, and pancreatic insufficiency. In the general population, 20% of bone loss occurs in the first five years after menopause. Dual-energy X-ray Absorptiometry (DXA) scans should be performed at least every two years for females with CF, especially those with osteopenia and osteoporosis. Increased activity, weight-bearing exercise, an increase in calcium and vitamin D, menopause hormone therapy (MHT), bisphosphonates, and denosumab can help build bone and/or reduce the rate of bone loss, thus improving bone mineral density. More research is needed to determine what treatments may be specifically appropriate for females with CF.
Use of Hormone Replacement Therapy in the CF population
[The benefits of hormone replacement therapy (HRT) in the general population, ages 50-59 years, include fewer bone fractures, improved diabetes control, and improvements in all-cause mortality. Yet there are also increased risks, including a higher risk for cerebrovascular accidents, pulmonary embolism, and deep vein thrombosis.[11] The Menopause Society’s 2022 hormone therapy position statement states:
The risks of hormone therapy differ depending on type, dose, duration of use, route of administration, timing of initiation, and whether a progestogen is used. Treatment should be individualized using the best available evidence to maximize benefits and minimize risks, with periodic reevaluation of the benefits and risks of continuing therapy. For women aged younger than 60 years or who are within 10 years of menopause onset and have no contraindications, the benefit-risk ratio is favorable for the treatment of bothersome vasomotor symptoms (VMS) and the prevention of bone loss. For women who initiate hormone therapy more than 10 years from menopause onset or who are older than 60 years, the benefit-risk ratio appears less favorable because of the greater absolute risks of coronary heart disease, stroke, venous thromboembolism, and dementia.[10]
Up until now, the risks and benefits of HRT have been extrapolated from the general population to the CF population.[12] Further studies are needed to determine the optimal approach for peri- and post-menopausal women with CF. For her part, Prochownik found that 75% of their participants with CF on HRT reported no change in their CF symptoms. Twenty-four of these participants were on estradiol only, while [15] participants were on estradiol and progesterone.[6,7] Contraindications for the use of HRT in females with CF include: a history of venous thromboembolism (blood clots in the vein), liver disease, and CFRD with vascular disease.[6] Females should consult with their physician(s) for alternatives to hormonal therapies, if needed.
There may be potential drug interactions between HRT and some CF medications. According to Fitzpatrick, CFTR modulators (except for lumacaftor) and azithromycin undergo hepatic metabolism. Ivacaftor, tezacaftor, and elexacaftor are metabolized by CYP3A, a group of enzymes that are part of the cytochrome P450 3A subfamily. They play a key role in metabolizing various drugs and other substances within the body.[13] Ivacaftor inhibits CYP3A and lumacaftor induces CYP3A. Inhaled therapies do not have significant absorption, and pancreatic enzymes are locally absorbed.[14]
Impact of Hormone Replacement Therapy (HRT)
HRT, also called hormone therapy or post-menopause hormone therapy, can help with night sweats, mood swings, hot flashes and reduced libido associated with menopause [2]. Options include estrogen-only therapy or estrogen–progestogen therapy (EPT) and patients should be well informed to weigh the benefits and potential risks [10]. HRT can be administered orally or topically with an intravaginal cream or patch. One concern about HRT is its effect on the liver. Some CF and transplant medications can be taxing on the liver and oral estrogen used to treat hot flashes also have a pronounced effect on the liver. Estrogen topical preparations avoid “the first-pass effect” of being primarily metabolized through the liver”[5].
Recent observational study has shown that there is an increased risk of breast cancer (or pre-invasive ductal carcinoma in situ) for women using combined HRT after >5 years of treatment. This risk increases with prolonged treatment…(and)… there was no increased risk of breast cancer seen for users of oestrogen-only therapy” [11,12]. Results from the Women’s Health Initiative (WHI) studies, which assessed the risks and benefits of HRT in postmenopausal (non-CF) women, indicate that [13,14]:
- women who took estrogen alone or estrogen plus progestin had a lower risk of hip and vertebral fractures than women who took placebo;
- women who took estrogen plus progestin had more vaginal bleeding that required assessment by endometrial biopsy than women who took placebo;
- women who took estrogen alone or estrogen plus progestin had an increased risk of urinary incontinence;
- women age 65 and older who took estrogen alone or estrogen plus progestin had an increased risk of developing dementia, women who took either combined hormone therapy or estrogen alone had an increased risk of stroke, blood clots, and heart attack [11,12];
- women who took estrogen alone had a lower risk of breast cancer than women who took placebo [15]
- women who took estrogen plus progestin were more likely to be diagnosed with breast cancer than women who took placebo and the risk of breast cancer was greater the longer women took the combined hormone therapy, but it decreased markedly when hormone use stopped [16];
- and in the initial study report, women taking combined hormone therapy had a lower risk of colorectal cancer than women who took placebo [17].
It is important to note that risks for the aforementioned diagnoses reduced when women stopped HRT [17].
HRT and Females who are Post-Transplant
Transplanted females with CF may have more complicated risk-benefit profiles for taking MHT than other females with CF. Providers and patients should consider any potential drug interactions with MHT, as well as between herbal medications and MHT. A woman’s past medical history should be considered when evaluating the suitability of prescribing MHT in females who are transplanted.
Researchers have shown that HRT improves women’s quality of life during perimenopause and postmenopause. It is best to use the lowest therapeutic dose for the shortest possible time. Longer durations of HRT can be indicated for persistent vasomotor symptoms, but shared decision-making and reevaluation are necessary. For women with genitourinary syndrome who do not have indications for HRT, and whose genitourinary symptoms are not helped by over-the-counter treatments, the Menopause Society recommends low-dose vaginal estrogen therapy or other therapies, like vaginal dehydroepiandrosterone or oral ospemifene.[10]
Non-hormonal menopause therapies are now available. Fezolinetant (Veozah), a non-hormonal therapy for VMS, was approved by the FDA in 2023. SSRIs/SNRIs, gabapentin, and oxybutynin can also be effective in reducing menopause symptoms.
While there are treatment options for MT, there is no cure except time.
- HRT might supplement estrogen and progesterone levels to ease the symptoms that occur in (peri)menopause, like hot flashes, night sweats, or sleep disruption [13].
- SSRIs (selective serotonin reuptake inhibitors) and SNRIs (serotonin and norepinephrine reuptake inhibitors) might help with depression and hot flashes. Dr. Cynthia Stuenke, a founding member of the North American Menopause Society and a professor and endocrinologist at the University of California, San Diego, School of Medicine, says, “While they’re not perfect, they can take the edge off and help enough so that women can get a better night’s sleep” [18].
- In 2015, a North American Menopause Society panel found that cognitive behavioral therapy and hypnosis were significantly effective in treating hot flashes. The same panel also found that popular herbal remedies (like black cohosh, dong quai and evening primrose) are “unlikely to help,” despite anecdotal reports that women find them helpful [18].
- Guided meditation and mindfulness to help with relaxation and mood swings.
- Regular exercise can help with weight gain, metabolism changes, mood issues and joint pain.
- To combat sleep disturbances, establish sleep habits and practices.
Are there Benefits to Menopause?
While there can be late life pregnancies in the perimenopause phase, some women experience a sexual resurgence and appreciate the freedom from menstrual cycles and contraceptives in menopause [19]. Support from other women and the ability to share stories can help women bond and deal with the changes they experience [18]. The National Women’s Health Information Center finds that society’s and women’s ideas about menopause might become more nuanced if more women were vocal about their menopause experience [18].
Mental Health and Menopause
Tsang has noted the most significant reported perimenopausal changes for women with CF were sleep disturbance and depression[6]. For its part, menopause research in the general population suggests that having a history of depression makes it more likely a woman will experience a depressive episode as she approaches menopause. Bromberger and Epperson (2018) recommend treating women for depressive symptoms experienced during this transitional phase and indicate that the rate of depression declines 2-4 years after the final menstrual period [7].
- Develop a strong support system to help you navigate the MT.
- Connect with others who have CF using social media and video conferencing to talk about menopause symptoms and strategies.
- Modulators can exacerbate anxiety and depression, which makes attending to your mental health even more important during the MT.
- Increase your physical activity and incorporate strength training to help counter bone loss during late perimenopause.
- To counter mood changes during perimenopause, consider taking up meditation, yoga, mindfulness, or journaling.

Peer to Peer Advice
- Try herbal supports, but check with your doctor before starting any supplements. Try Melissa Lemon Balm, which showed improved sexual function after menopause [See the Sexual Function chapter][20].
- Experiment with different lubricants that are glycerine, paraben and petrochemical free to help with vaginal dryness, tearing and dyspareunia [See the Sexual Function chapter]
- Consider treatments for vaginal rejuvenation using energy-based nonsurgical procedures on vaginal tissue that have been used to improve vaginal dryness or vaginal atrophy (thinning of the vaginal wall) during perimenopause or postmenopause. You should find a qualified healthcare physician for this treatment. Cleveland Clinic information on energy based treatments and vaginal rejuvenation.
- Consider vaginal dilator therapy that can be used at home to stretch the vagina because vaginal atrophy is associated with menopause. However, a recent study showed that there were no clinically proven standardized protocols or formalized guidelines to give to patients about how to best use their dilators. Larger long-term future studies are required to assess effectiveness [21]. Consult your gynecologist or urologist for more information.
- Find a network of perimenopausal and menopausal women who share their experiences, which can be helpful [18].
- Seek information to cope with menopause. The National Women’s Health Information Center has a section on menopause and perimenopause [18]. The North American Menopause Society (NAMS) is another option.
- Remembering that menopause is a normal physiological life transition can help women cope and view some changes as positive [18].
Works Cited
- Gatenby C, Simpson P. Menopause: Physiology, definitions, and symptoms. Baillières Best Pract Res Clin Endocrinol Metab. 2024;38(1):101855. doi:10.1016/j.beem.2023.101855
- Harlow SD, Gass M, Hall JE, et al. Executive Summary of the Stages of Reproductive Aging Workshop + 10: Addressing the Unfinished Agenda of Staging Reproductive Aging. J Clin Endocrinol Metab. 2012;97(4):1159-1168. doi:10.1210/jc.2011-3362
- Harvard Health Online. Perimenopause: Rocky road to menopause. August 9, 2022. Accessed June 22, 2025. https://www.health.harvard.edu/womens-health/perimenopause-rocky-road-to-menopause
- Office on Women’s Health. Menopause Basics. https://womenshealth.gov/menopause/menopause-basics
- Tsang A, Thompson K, Paul R, Tullis E. Perimenopause in CF: Assessment of Onset and Symptomatology: 572. Pediatr Pulmonol. 2009;44:417.
- Jain R. S03.2 Hormonal Effects of Aging and Menopause in Females with CF. In: Golden Girls: Care Considerations for the Aging CF Female; 2024.
- Prochownik K, Jain R, Taylor-Cousar JL, et al. Menopause in people with cystic fibrosis. Menopause. Published online January 31, 2023. doi:10.1097/GME.0000000000002155
- Tehrani FR, Amiri M. The association between chronic diseases and the age at natural menopause: a systematic review. Women’s Health. 2021;61(10):917-936. doi:10.1080/03630242.2021.1992067
- Gold EB, Crawford SL, Avis NE, et al. Factors Related to Age at Natural Menopause: Longitudinal Analyses From SWAN. Am J Epidemiol. 2013;178(1):70-83. doi:10.1093/aje/kws421
- Faubion S, Crandall C, Davis L, et al. The 2022 hormone therapy position statement of The North American Menopause Society. Menopause N Y N. 2022;29(7):767-794. doi:10.1097/GME.0000000000002028
- Stuenkel C, Davis S, Gompel A. Treatment of symptoms of the menopause: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2015;100(11):3975-4011.
- West NE, Kazmerski TM, Taylor‐Cousar JL, et al. Optimizing sexual and reproductive health across the lifespan in people with cystic fibrosis. Pediatr Pulmonol. 2022;57(S1):S89-S100. doi:10.1002/ppul.25703
- Shannon M. Drug Interactions. In: Clinical Management of Poisoning and Drug Overdose. 4th edition; 2007:97-104.
- Fitzpatrick L. S03.3- Bridging the Gap: Understanding Drug Interactions in Medications & Herbal Treatments Utilized in Mature CF Women. In: S03–Golden Girls: Care Considerations for the Aging CF Female; 2024.
Additional articles:
- West, Natalie E., et al. “Optimizing Sexual and Reproductive Health across the Lifespan in People with Cystic Fibrosis.” Pediatric Pulmonology, vol. 57, no. S1, 2022, pp. S89-100. https://onlinelibrary.wiley.com/doi/10.1002/ppul.25703
- Frayman, Katherine B., and Susan M. Sawyer. “Sexual and Reproductive Health in Cystic Fibrosis: A Life-Course Perspective.” The Lancet Respiratory Medicine, vol. 3, no. 1, 2015, pp. 70–86, https://doi.org/10.1016/S2213-2600(14)70231-0.
- Jain, Raksha, et al. “Challenges Faced by Women with Cystic Fibrosis.” Clinics in Chest Medicine, vol. 42, no. 3, 2021, pp. 517–30. https://doi.org/10.1016/j.ccm.2021.04.010.
- Tsang AO, Thompson K, Paul R, Tullis E. Pediatric Pulmonology. 2009; 44:417. https://oce.ovid.com/article/01445490-200909001-00650
Free Printable PDF Download
Want a free printable PDF download of this section for your use in clinic? Just give us your name and email address below to get your download link. This will not add you to our email list.