Incontinence
The involuntary release of urine or fecesCFReSHC CF-SRH Resource Guide by Patients for Providers and Patients
Introduction
Studies indicate that patients with cystic fibrosis (CF) experience pelvic incontinence (PI) at higher rates than the general population [1]. There are five common forms of incontinence: stress, urge, overflow and fecal.
Stress
Occurs with sudden pressure on the bladder (coughing, laughing sneezing, exercising)
Urge
Occurs with strong sudden urge to void; overactive bladder
Mixed
A combination of urge and stress urinary incontinence (UI) symptoms
Overflow
Occurs with loss of bladder muscle control; incomplete emptying of bladder/retention of urine
Fecal
Inability to control bowel movements; can occur with the passing of gas
Urinary incontinence (UI) affects approximately 30-69% of the female CF population, with between 80-100% of women over the age of 35 [2,3]. Of those women, almost half do not mention their UI to any provider. They therefore do not receive a diagnosis and/or treatment for the issue [2]. A CFReSHC snap poll indicated that 22 out of 24 female respondents self-identified as having urinary and/or fecal incontinence [4]. Incontinence in CF often goes unreported and under treated for three reasons: 1) patients feel embarrassed discussing urine and/or fecal leakage; 2) CF providers are unaware of these experiences; and 3) CF providers consider incontinence outside their medical expertise [2,3]. Research has found that other barriers to seeking treatment for UI among women, in general (not just those with CF), include having a male doctor, feeling they are too young to experience UI, and having not experienced childbirth [5]. As a result, patients suffer in silence, unaware that treatment options exist.
While UI is the more common form of pelvic incontinence in CF, some patients do experience fecal incontinence. Fecal incontinence is the occasional leakage of stool while passing gas or the complete loss of bowel control. Fecal incontinence is more common among people who suffer from chronic constipation, a symptom that many people with CF experience [6]. Research among youth with chronic constipation has identified an association with pain, stress, and fecal incontinence, which negatively impacts health-related quality of life [6]. The prevalence of fecal incontinence is unknown in the CF population, however, and thus warrants further research.
- Are you experiencing changes in your urinary and bowel habits, like the urge to urinate at night or urinating multiple times in an hour?
- Women with CF can have urine and/or feces leak when they cough, laugh or do PFTs. What urinary or bowel changes have you noticed?
- Have you ever been treated for incontinence before? If you experience incontinence would you like a referral to a specialist that can help manage that?
PFT Technician to Patient:
- PFT Technician: Ask your patient if they experience incontinence during airway clearance, coughing, or exerting on their PFT.
- PFT Technician: Do you need to use the bathroom before doing your PFT ?
To Any Provider
- What resources can you offer to help me with incontinence?
- I noticed that I am having accidents when I ________________. Is there a provider you recommend who could help me with this problem?
- What can I do now to prevent getting incontinence in the future?
What to know about Incontinence
UI symptoms can range from infrequent episodes with a few drops of urine, to more severe symptoms, with leakage occurring several times a day and with enough leakage to require wearing a pad or requiring a clothing change.
CF is characterized by increased cough, altered respiratory mechanics and abnormal posture [2]. Typically, pelvic muscles support the pelvic organs and bladder like a hammock, but the frequent, intense coughing can weaken the muscles surrounding the urethra, vaginal opening, and anus, making them less effective [1]. This is known as pelvic floor dysfunction. In comparing CF coughing patterns to healthy patients with a cold, Dodd and Langman (2012) found that CF coughs have increased intensity and duration, leading to potential incidence of incontinence [2].
Another possible reason for an increased incidence of UI in women with CF is that patients tend to contract their pelvic floor muscles during frequent coughing. They could, therefore, have the tendency to keep pelvic floor muscles chronically contracted, thus weakening them [7].
The occurrence of UI is not directly linked to poor lung function, BMI, CFRD, or the presence of a gastric tube [8]. Furthermore, both child-bearing and non-childbearing women with CF experience UI.
Impact upon Women’s Lives:
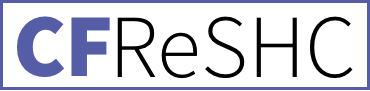
Incontinence affects both women’s clinic behaviors and their daily lives in numerous ways. For example, patients may not exhale fully during pulmonary function testing to avoid the pressure placed on the pelvic floor muscles in an effort to avoid incontinence. This strategy to avoid urinary incontinence can compromise the “assessment and management of their lung disease” [2]. Likewise, patients may limit airway clearance to avoid leakage. They might also abstain from or reduce exercise, intimacy with a partner, or other potential triggers to avoid leakage, especially if those activities occur in public. Women may also urinate prior to need, limit fluid intake, or change their level of activity so they can stay close to a bathroom [5].
Females’ body image and self-esteem can suffer from UI. Nygaard et al. state that an association between depression and incontinence exists amongst middle-aged women [9]. In their exploratory study of middle aged, partnered women (n=57), Saiki and Meize-Grochowski found that psychological health, relationship satisfaction, and relationship dynamics were correlated, no matter the severity of their symptoms [10]. More specifically, UI can cause women to experience a loss of desire, less lubrication, and less sexual satisfaction. Fear of coital urinary incontinence can lead to less frequent sexual activity, more avoidance behaviors, dyspareunia, and abstinence in women with UI [11]. [see the Sexual Function chapter]. UI can also cause women to avoid achieving orgasm for fear of leaking [6]. These behaviors can affect partners and strain intimate relationships, although women who experience them tend to express larger worries than their partners [10, 12-14].
For women with CF, chronic contraction of the pelvic floor during coughing can lead some patients to tighten their vagina, leading to painful sex and other vaginal health conditions. Yet, like other women, the barriers that prevent self-reporting of UI, including stigma, shame, and embarrassment, as well as “perceived bother,” may also prevent patients from seeking treatment for incontinence [5]. In 2001, Orr suggested providers need to develop a “practical and sensitive approach” to address incontinence as part of their routine CF management, but this approach has not yet been widely implemented [3]. With provider and patient education, pelvic incontinence screening for CF patients can increase [3,7,15]. Such efforts are needed because leakage can become progressive and chronic, worsening quality of life.
Treatment options
According to Physical Therapist Beth Taylor, diagnosing pelvic floor dysfunction involves an assessment of symptoms, an internal exam, incontinence education and developing a plan of care [7]. Being overweight, ingesting caffeine, eating spicy food, and drinking alcohol can trigger urinary incontinence (UI) in the general population, as can declining estrogen as females age and enter menopause [3].
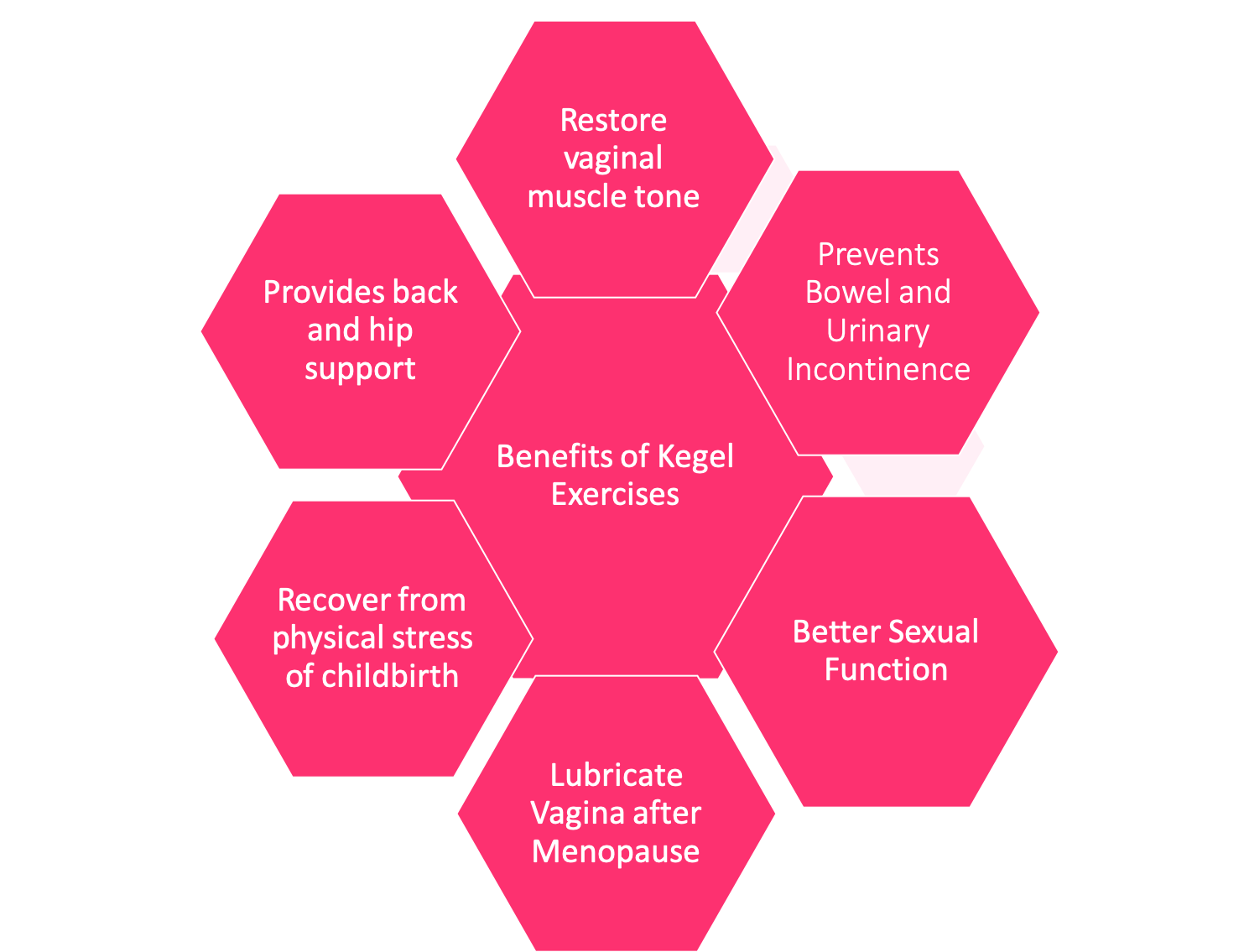
Referral to a gynecologist, urogynecologist, or pelvic floor specialist for patients affected by UI can help expedite treatment. Successful treatment often teaches patients how to properly do “kegel” exercises. Kegels help the patient locate and engage their pelvic floor muscles so that when UI occurs, they can contract these muscles to minimize leakage while coughing and during airway clearance [16]. For women experiencing chronic contraction of pelvic floor muscles, treatment with reverse Kegels might be an option; proper diagnosis and treatment, preferably by a pelvic floor specialist, is necessary [9].
Additionally, physical therapists recommend exercises focusing on improved posture to help relieve UI [15]. Various forms of exercise may also help improve incontinence, including yoga, pilates, and weight training. Medication, biofeedback, electrical stimulation, bladder training, and surgery are all options if PT fails to resolve UI. However, treatment options vary based on the individual patient; what works for one woman may not work for another. This short instructional video of Pilates exercises that address UI may be helpful.
Gaps in knowledge and treatment
There is no data yet about how reduced cough by patients on CFTR modulators will impact incontinence incidence and prevalence rates. Despite a potential decrease in the incidence rate of urinary incontinence (UI) in patients with CF, these patients may still have weakened pelvic floor muscles. UI could therefore still be present and may require treatment through postural changes, medications, and physical therapy. In addition, there is no data that assesses the prevalence of fecal incontinence (FI); particularly whether it is more common when patients are on antibiotics and experience loose stools.
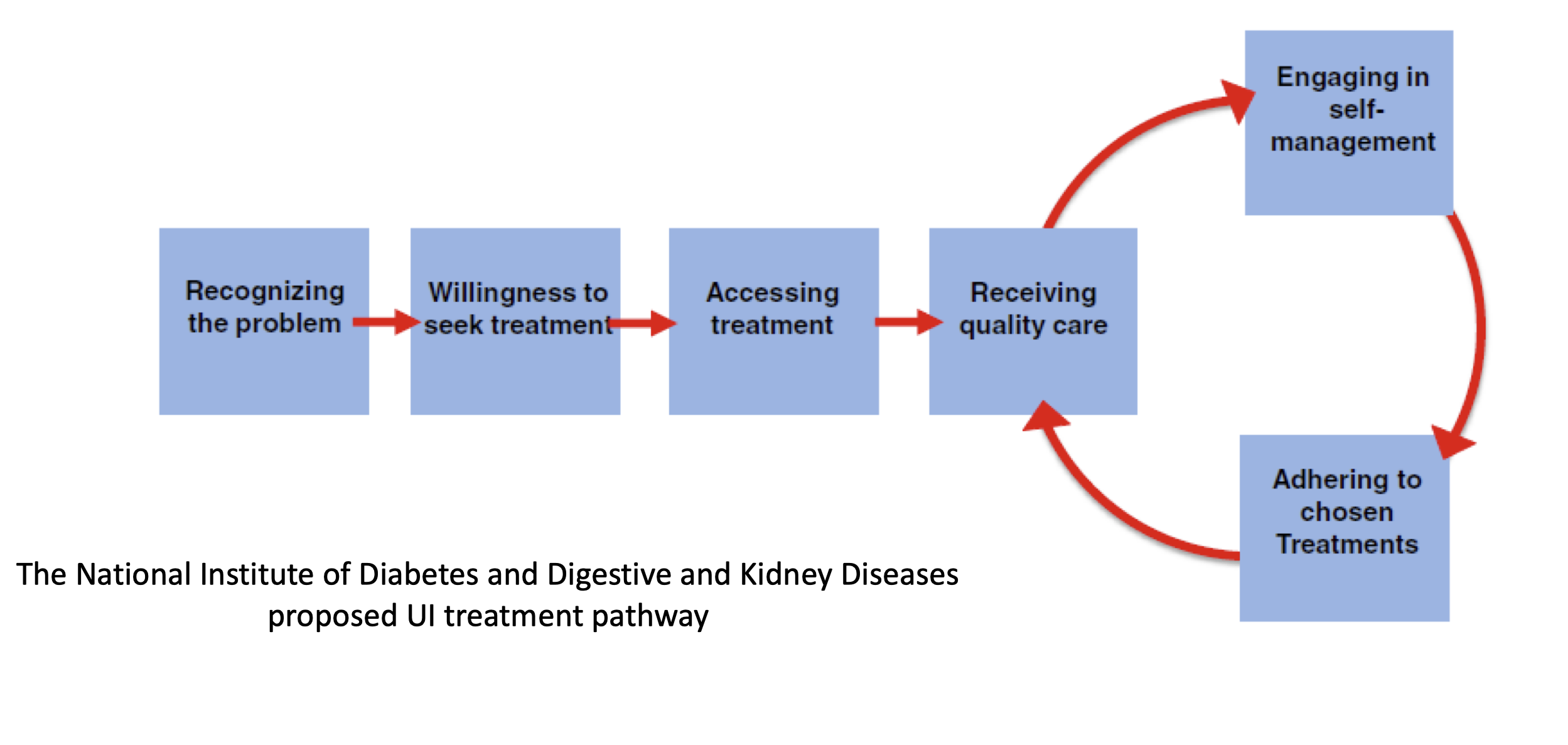
Several years ago, the National Institute of Diabetes and Digestive and Kidney Diseases convened a workshop spanning two sessions where experts proposed a UI treatment pathway. The pathway (Figure 1) consists of 5 steps women must navigate to successfully address their symptoms.
Operationalizing this pathway through routine discussion and assessment of UI in CF clinical care, provision of psychosocial support, and development of a robust referral system could improve access to UI care for female patients. However, a lack of incontinence management in CF clinical care persists.


Peer to Peer Advice
- It’s possible to see a pelvic floor physical therapist for incontinence treatment much like doing rehab for a knee injury.
- Using pads specifically designed for incontinence can help if you have symptoms. [Note: incontinence pads are different from menstruation pads or panty liners.]
- After you urinate, stay on the toilet, lean forward and even rock back and forth to make sure all urine is released. Sometimes we think we are done urinating, but the bladder does not empty completely.
- Do not wait to use the restroom but also do not force out urine.
- Download the Squeezy CF app to get information and exercises that may help you (There is a cost for this application).
- Use a device that monitors your Kegels to make sure they are effective. There are free apps to help with Kegel exercises.
- Using the toilet while coughing can help avoid embarrassing urine and/or stool leakage.
- See a urogynecologist to learn if you could benefit from a surgical repair to your bladder or urethra, which can improve function when the pelvic floor has been weakened from chronic coughing.
Resource Links
Works Cited
- Neemuchwala F, Ahmed F, Nasr SZ. Prevalence of pelvic incontinence in patients with cystic fibrosis. Global Pediatric Health. 2017;4:2333794X17743424. https://journals.sagepub.com/doi/full/10.1177/2333794X17743424. doi: 10.1177/2333794X17743424.
- Dodd ME, Langman H. Urinary incontinence in cystic fibrosis. Journal of the Royal Society of Medicine. 2005;98 Suppl 45(Suppl 45):28-36. https://www.ncbi.nlm.nih.gov/pubmed/16025765.
- Orr A, McVean RJ, Webb AK, Dodd ME. Questionnaire survey of urinary incontinence in women with cystic fibrosis. BMJ. British medical journal (Clinical research ed.). 2001;322(7301):1521. https://www.ncbi.nlm.nih.gov/pubmed/11420273.
- CF Reproductive and Sexual Health Collaborative. CFReSHC Snap Poll on Incontinence. 7.27.2020.
- Norton J, Dodson J, Newman D, et al. Nonbiologic factors that impact management in women with urinary incontinence: Review of the literature and findings from a national institute of diabetes and digestive and kidney diseases workshop. Int Urogynecol J. 2017;28(9):1295-1307. https://www.ncbi.nlm.nih.gov/pubmed/28674734. doi: 10.1007/s00192-017-3400-x.
- Klages KL, Berlin KS, Silverman AH, et al. Empirically derived patterns of pain, stooling, and incontinence and their relations to health-related quality of life among youth with chronic constipation. Journal of pediatric psychology. 2017;42(3):325-334. https://www.ncbi.nlm.nih.gov/pubmed/27474732. doi: 10.1093/jpepsy/jsw068.
- Taylor B. CFReSHC patient task force meeting presentation on incontinence and CF. 12.10.2019.
- Frayman KB, Kazmerski TM, Sawyer SM. A systematic review of the prevalence and impact of urinary incontinence in cystic fibrosis. Respirology. 2018;23(1):46-54. https://onlinelibrary.wiley.com/doi/abs/10.1111/resp.13125. doi: 10.1111/resp.13125.
- Nygaard I, Turvey C, Burns TL, Crischilles E, Wallace R. Urinary incontinence and depression in middle-aged United States women. Obstetrics & Gynecology. 2003;101(1):149-156. http://dx.doi.org/10.1016/S0029-7844(02)02519-X. doi: 10.1016/S0029-7844(02)02519-X.
- Saiki L, Meize-Grochowski R. Urinary incontinence and psychosocial factors associated with intimate relationship satisfaction among midlife women. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2017;46(4):555-566. http://dx.doi.org/10.1016/j.jogn.2017.02.003. doi: 10.1016/j.jogn.2017.02.003.
- Duralde ER, Rowen TS. Urinary incontinence and associated female sexual dysfunction. Sexual Medicine Reviews. 2017;5(4):470-485. https://search.proquest.com/docview/1931253113. doi: 10.1016/j.sxmr.2017.07.001.
- Kizilkaya Beji N, Yalcın O, Ayyildiz EH, Kayir A. Effect of urinary leakage on sexual function during sexual intercourse. Urologia Internationalis. 2005;74(3):250-255. https://www.karger.com/Article/Abstract/83558. doi: 10.1159/000083558.
- Coyne KS, Margolis MK, Jumadilova Z, Bavendam T, Mueller E, Rogers R. Overactive bladder and women’s sexual health: What is the impact? The Journal of Sexual Medicine. 2007;4(3):656-666. https://doi.org/10.1111/j.1743-6109.2007.00493.x. doi: 10.1111/j.1743-6109.2007.00493.x.
- McPheters JK, Sandberg JG. The relationship among couple relationship quality, physical functioning, and depression in multiple sclerosis patients and partners. Families, Systems, & Health. 2010;28(1):48-68. https://search.datacite.org/works/10.1037/a0018818. doi: 10.1037/a0018818.
- von Berg K. CFReSHC patient task force meeting presentation on incontinence and cystic fibrosis. 5.30.2018.
- Blackwell K, Malone PSJ, Denny A, Connett G, Maddison J. The prevalence of stress urinary incontinence in patients with cystic fibrosis: An under-recognized problem. Journal of Pediatric Urology. 2005;1(1):5-9. http://dx.doi.org/10.1016/j.jpurol.2004.07.001. doi: 10.1016/j.jpurol.2004.07.001.
Free Printable PDF Download
Want a free printable PDF download of this section for your use in clinic? Just give us your name and email address below to get your download link. This will not add you to our email list.